Execution of Distal Initiation (SLR-DI):
- Patient is in supine lying position
- The examiner flexes the patient’s knee and hip to create slack in the dura mater
- Then the ankle is dorsiflexed for distal pre-tension of the sciatic nerve
- From this position the examiner passively extends the leg and passively flexes the hip while maintaining dorsiflexion until symptoms occur
- Then, the patient flexes the neck to achieve maximal tension of the dura
- At last, the examiner releases the dorsiflexion to allow the dura to move into cranial direction towards the starting position
Execution of Proximal Initiation (SLR-PI):
- Patient is in supine lying position
- The examiner flexes the patient’s knee and hip to create slack in the dura mater
- Then the patient is asked to flex the head and neck in order to create pre-tension of lumbosacral plexus in cranial direction
- From this position the examiner dorsiflexes the patient’s ankle, extends the leg and passively flexes the hip while maintaining dorsiflexion until symptoms occur. This movement creates maximal tension at the dura, while the distal movement of the dura is limited due to the cranial pre-tension
- At last, the patient is asked to extend the head and neck again which reduces cranial tension and lets the dura move distally
Explanation:
The distal and proximal initiation of the Straight Leg Raise Test (SLR) can be used to distinguish between primary disc-related disorders (disc protrusion, prolapse, extrusion, which exert direct pressure on the nerve roots) and secondary disc-related disorders (due to decreased intervertebral space because of reduced disc height and bulging), such as epidural adhesions, nerve-root compression syndrome (NRCS) or intermittent neurogenic claudication (INC).
While in primary disc-related disorders the provocation is maximal during maximal dural tension, the provocation in secondary disc-related disorders is direction-specific. In these cases, provocation will occur due to loss of dural sleeve mobility associated with fibrosis or the compression of the nerve roots inflammatory focus.
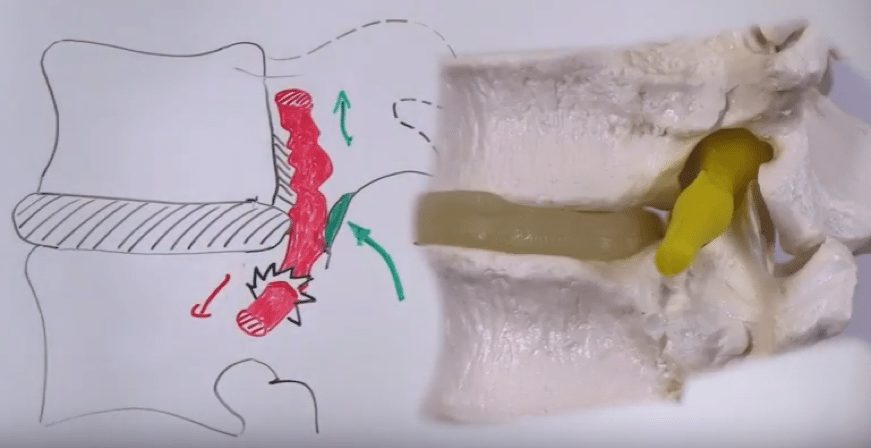
Imagine for example that your patient suffers from compression of an irritated nerve root between a degenerative disc bulge anterior and a hypertrophic ligamentum flavum posterior: Here, the pain will increase with distal movement and it will decrease with proximal movement. This is due to the reason that distal movement will translate the root’s irritable focus through the narrowed path.
Therefore, pain in secondary disc-related disorders is maximal with distal initiation and will decrease as soon as neck flexion is added, because the nerve’s irritable focus is moved into cranial flexion again. Pain will disappear completely, as soon as dorsiflexion is released, which lets the nerve travel cranially even further.
With the proximal initiation, pain is only felt during the last step when the proximal pre-tension is released by head and neck extension, which allows the lumbosacral plexus to move distally.
| Test | Primary disc-related disorders (Protrusion, Prolapse, Extrusion) | Secondary disc-related disorders (Epidural adhesions, NRCS, INC) |
| SLR-DI | ||
| Ankle DF+SLR | Mild/Moderate pain provocation | Maximal pain |
| Chin Tuck+Neck Fl. | Maximal pain | Less pain |
| Ankle PF | Less pain | No pain provocation |
| SLR-PI | ||
| Chin Tuck+Neck Fl. | No pain provocation | No pain provocation |
| Neck Flexion | Maximal pain | No pain provocation |
| Return head to mat | Less pain | Maximal pain |
| Study | Reliability | Sn | Sp | LR+ | LR- |
| Sizer et al. (2002) | NA | NA | NA | NA | NA |
| Comment: While these different build-ups of the SLR use sound structural clinical reasoning, no validity studies have confirmed or rejected this concept yet. | |||||
![]()